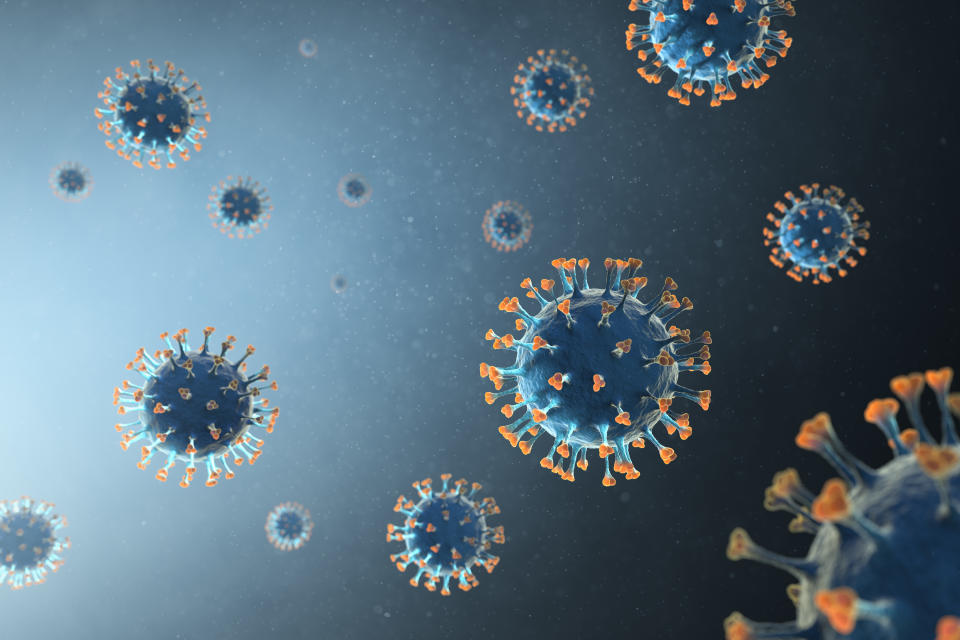
Russia's coronavirus vaccine produces immune response and no safety concerns, early research suggests

Early research suggests Russia’s controversial coronavirus vaccine is safe and produces an immune response.
In August, the nation became the first in the world to approve a jab following less than two months of human testing.
President Vladimir Putin announced the vaccine was officially registered with the Russian Health Ministry after it brought about “stable” immunity “quite effectively”, adding one of his daughters had been immunised and was doing well.
Experts expressed concern over the “rather little detail” Russian officials had released, with one warning a “less than safe and effective” vaccine could exacerbate the world’s “current problems insurmountably”.
Read more: Steroids could cut risk of death by a fifth in critically-ill COVID patients
A trial published in the prestigious medical journal The Lancet has since revealed, however, there were no serious safety concerns up to 42 days after the jab was administered.
The vaccine candidate also brought about an immune response within 21 days during a second trial.
One expert called the studies “encouraging but small”. While its “immunogenicity bodes well”, the vaccine’s ability to prevent infection or severe illness “has not yet been shown”, he added.

‘Teach the immune system to attack the virus’
A team of Russian scientists analysed a frozen and freeze-dried formulation of the vaccine candidate.
The team envision the frozen formulation will one day be rolled out across existing vaccine supply chains, while the more stable freeze-dried version was developed for hard-to-reach regions.
Both formulations of the jab are based on adapted strains of the adenovirus. This usually causes the common cold but has been modified to express the coronavirus’ spike protein, which it uses to enter cells.
Read more: Man with coronavirus develops testicular swelling
Scientists from the University of Oxford also had preliminary success with their adenovirus-based jab, which brought about an immune response up to day 56.
To test the Russian vaccine’s safety as part of a phase 1 trial, four groups of nine healthy volunteers were given either the frozen or freeze-dried jab.
One group received a frozen version of an adenovirus strain called type 26, while another had type five. The remaining two groups were given the freeze-dried formulation of type 26 or type five.
To gauge the formulations’ efficacy in a phase 2 trial, 40 volunteers had either a frozen or freeze-dried type 26 adenovirus-based jab, followed by a type five booster three weeks later.
Explaining why both type 26 and type five were required, lead author Dr Denis Logunov from the NF Gamaleya National Research Centre for Epidemiology and Microbiology said: “When adenovirus vaccines enter people’s cells, they deliver the [coronavirus] spike protein genetic code, which causes cells to produce the spike protein.
“This helps teach the immune system to recognise and attack the virus.
Read more: Britons struggled to maintain their weight during lockdown
“To form a powerful immune response against [the coronavirus], it is important a booster vaccination is provided.
“However, booster vaccinations that use the same adenovirus vector might not produce an effective response, because the immune system may recognise and attack the vector.
“For our vaccine, we use two different adenovirus vectors in a bid to avoid the immune system becoming immune to the vector.”
‘Unprecedented measures’ to develop coronavirus vaccine
Preliminary results of the phase 1 trial have revealed both formulations of the vaccine were “safe and well tolerated” over the 42 days.
More than half (58%) of the volunteers experienced pain at the site of the injection, while 50% had a temperature and just over two in five (42%) reported a headache – all of which are common with vaccines like these, according to the scientists.
No serious adverse events were detected, they added.
When it comes to an immune response, all of the phase 2 trial’s 40 volunteers produced antibodies against the coronavirus’ spike protein.
Antibodies are released by the immune system when it encounters a pathogen, like a virus. They then lock onto the virus’ surface, “marking” it for destruction by other immune cells.
Neutralising antibodies – which block the virus from entering cells – were detected in all of the 40 participants, but only 61% of those in the phase 1 trial who received the type 26 strain.
After looking at the plasma of more than 4,000 people who recovered from a mild coronavirus infection, the scientists concluded “the antibody responses appear to be higher in people vaccinated”.
Read more: Pregnant women less likely to develop fever with coronavirus
The results also revealed a T-cell response occurred in the 40 participants within 28 days.
T-cells can be helper, which stimulate antibody production and assist in the development of killer T-cells. The latter then directly destroy body cells that have already been infected by a pathogen.
The 40 volunteers’ helper and killer cells increased by 2.5% and 1.3%, respectively, following vaccination with the frozen formulation. After the freeze-dried jab, the helper and killer cells rose by 1.3% and 1.1%, respectively.
The scientists concluded using different adenovirus strains appears to be an “effective approach to elicit a robust immune response”, but added research is required to confirm this.
They noted their studies were relatively short with no placebo group, with this being considered a gold-standard of clinical research.
Although the scientists recruited volunteers aged between 18 and 60, most of the participants were relatively young, they added.
“Unprecedented measures have been taken to develop a COVID-19 [the disease caused by the coronavirus] vaccine in Russia,” said research author Professor Alexander Gintsburg, from the NF Gamaleya National Research Centre.
“Preclinical and clinical studies have been done, which has made it possible to provisionally approve the vaccine under the current Decree of the Government of the Russian Federation of 3 April 2020 no 441.”
The scientists next plan to test the vaccine formulations on “40,000 volunteers from different age and risk groups”.
‘So far, so good’
Writing in a linked Lancet comment, Dr Naor Bar-Zeev from Johns Hopkins University – who was not involved in the research, said: “Similar to these studies before it, [the scientists’] studies are encouraging but small.
“The immunogenicity bodes well, although nothing can be inferred on immunogenicity in older age groups, and clinical efficacy for any COVID-19 vaccine has not yet been shown.
“Safety outcomes up to now are reassuring, but studies to date are too small to address less common or rare serious adverse events.
“Unlike clinical trials of therapeutics, in which safety is balanced against benefit in patients, vaccine trials have to balance safety against infection risk, not against disease outcome.
“Since vaccines are given to healthy people and during the COVID-19 pandemic potentially to everyone after approval following phase 3 trials, safety is paramount.”
Russia’s deputy prime minister Tatyana Golikova announced in August the vaccine will be rolled out to the public as part of a mass campaign in early 2021.
“Licensure in most settings should depend on proven short-term and long-term efficacy against disease, and more complete safety data,” said Dr Bar-Zeev.
“In view of the ongoing painful toll of the COVID-19 pandemic and its magnitude, the more vaccine candidates that have successful early results the better.
“Ultimately, all vaccine candidates will need to show safety and prove durable clinical efficacy (including in groups at greater risk) in large randomised trials before they can be put into widespread use.”
Dr Michael Head from the University of Southampton agreed, adding: “This manuscript confirms some of the public statements from a few weeks ago, namely that this appears to be a promising vaccine candidate.
“Phase 1 and phase 2 trials have been carried out, and there is sufficient reason to scale up into much larger phase 3 trials. That would be the right way to go about vaccine development R&D.
“Concerns do remain around some of the previously-made ambiguous comments that this vaccine is about to be formally approved and licensed.
“At this stage, we do not know if the vaccine actually works – that is what the phase 3 trials will tell us.
“Public confidence in any licensed vaccine is vital, and suggestions from both Russia and the USA that a vaccine may be fast-tracked without the proper research having taken place are problematic.”
Professor Ian Jones from the University of Reading added adenovirus-based vaccines in general are “safe and generate an immune response to the [coronavirus] protein that is incorporated”.
“What everyone wants to know is if this translates the protection in the field,” he said.
Professor Brendan Wren from the London School of Hygiene & Tropical Medicine added: “The report is a case of ‘so far so good’, but immunological responses may not necessarily evoke protection and further investigation is needed on the effectiveness of this vaccine for prevention of COVID-19.”
 Yahoo Sport
Yahoo Sport